Brain neuropathology similar to Alzheimer’s patients was found in stranded dolphin brains, serving as strong evidence that cyanobacterial exposure is a risk factor in the development of neurological disease in both dolphins and humans.
One of the most heartbreaking occurrences for nature lovers is to discover a beached marine mammal such as a dolphin or whale. Some are discovered after they have died, giving rise to the question: Why do dolphins and whales become stranded on shore in the first place?
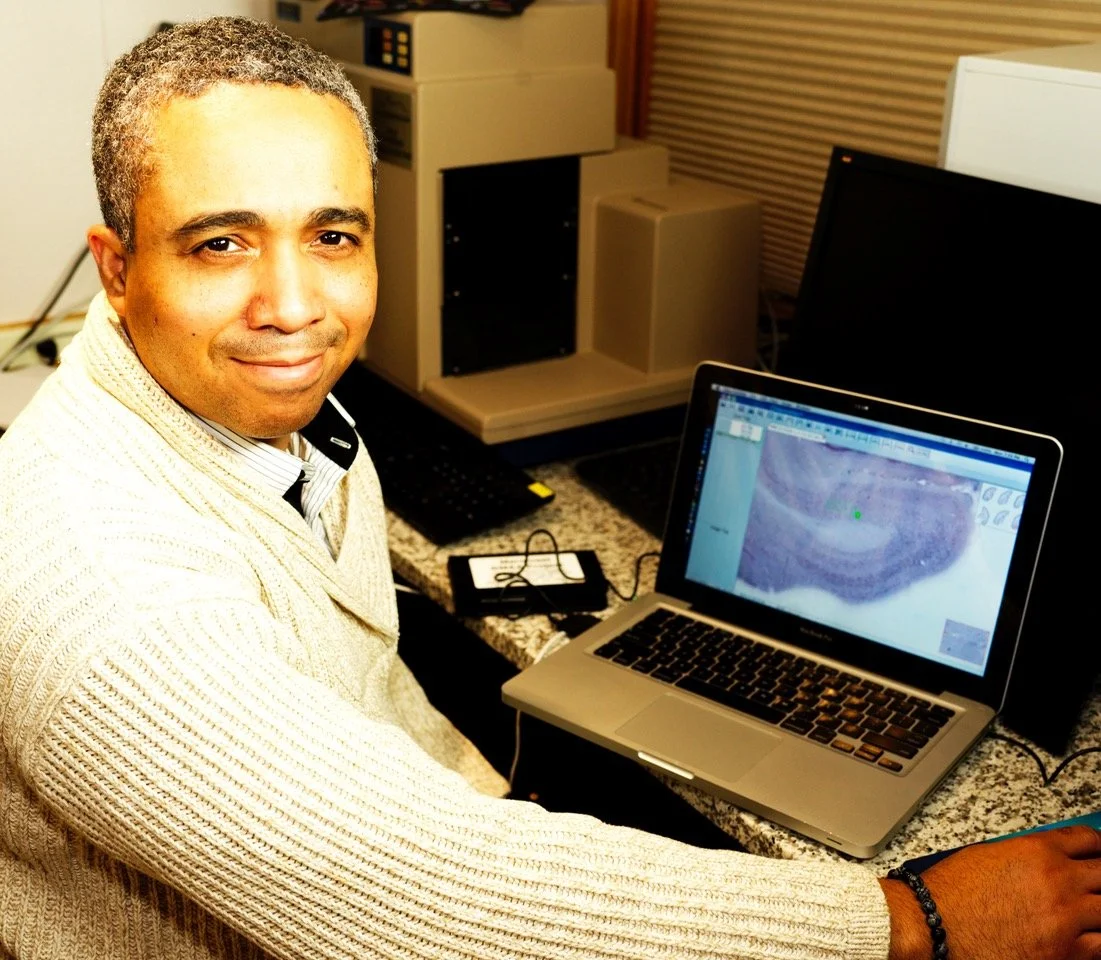
Dr David Davis examines brain samples from dolphins.
A group of scientists ranging from Wyoming to Florida has come up with an unusual hypothesis: Just as some adult humans with dementia are occasionally found wandering far from their homes, perhaps dolphins become similarly disoriented if suffering from a form of Alzheimer’s disease.
Prior studies of villagers on the island of Guam by researchers at the Brain Chemistry Labs in Jackson, Wyoming showed that chronic dietary exposure to cyanobacterial toxins are associated with misfolded tau proteins and amyloid plaques characteristic of Alzheimer’s disease. The cyanobacterial toxin BMAA and related isomers, known as 2,4-DAB and AEG, have been found to be extremely toxic to neurons. BMAA triggers Alzheimer’s-like neuropathology and cognitive loss in experimental animals. These toxins can be biomagnified up the food chain in the marine ecosystem.
In the case of marine mammals, a study of twenty common bottlenose dolphins stranded in the Indian River Lagoon in eastern Florida showed that their brains contained BMAA and its isomers, particularly 2,4-DAB. Dolphins stranded during the summer cyanobacterial bloom season contained 2,900 times the concentration of 2,4-DAB than those from non-bloom seasons.
It appears that Alzheimer’s-type neuropathology and disorientation in these dolphins was the result of chronic exposure to toxic molecules produced by cyanobacteria.
“Since dolphins are considered environmental sentinels for toxic exposures in marine environments,” Dr. David Davis at the Miller School of Medicine explains, “there are concerns about human health issues associated with cyanobacterial blooms.”
Senior Scientist, Dr Sandra Banack at the triple quadrupole mass spectrometer at the Brain Chemistry Labs.
In 2024, Miami Dade County had the highest prevalence of Alzheimer’s disease in the United States. “Although there are likely many paths to Alzheimer’s disease, cyanobacterial exposures increasingly appear to be a risk factor,” adds Dr. Davis.
“Among Guam villagers, we found that exposure to cyanobacterial toxins appeared to trigger neurological disease,” said Dr. Paul Alan Cox, Executive Director of the Brain Chemistry Labs in Jackson.
————
This research paper, "Alzheimer's disease signatures in the brain transcriptome of Estuarine Dolphins," was published in the Nature journal Communication Biology.