A blood test to diagnose amyotrophic lateral sclerosis (ALS) could be widely available within two years.
Currently, ALS is diagnosed through a clinical examination by a neurologist but distinguishing it from other neurological diseases requires tracking symptom progression.
This is problematic, as the average survival time in ALS is approximately three years, meaning many patients deteriorate significantly before receiving a definitive diagnosis.
Initial misdiagnosis rates range as high as 68%, delaying treatment and causing patients to be passed between specialists, increasing anxiety, unnecessary interventions, and costs.
A simple blood test for ALS would be a game-changer. It would speed up diagnosis, reduce anxiety, lower costs, and support the development of new drugs. Given the high misdiagnosis rate, a negative result would also be highly valuable.
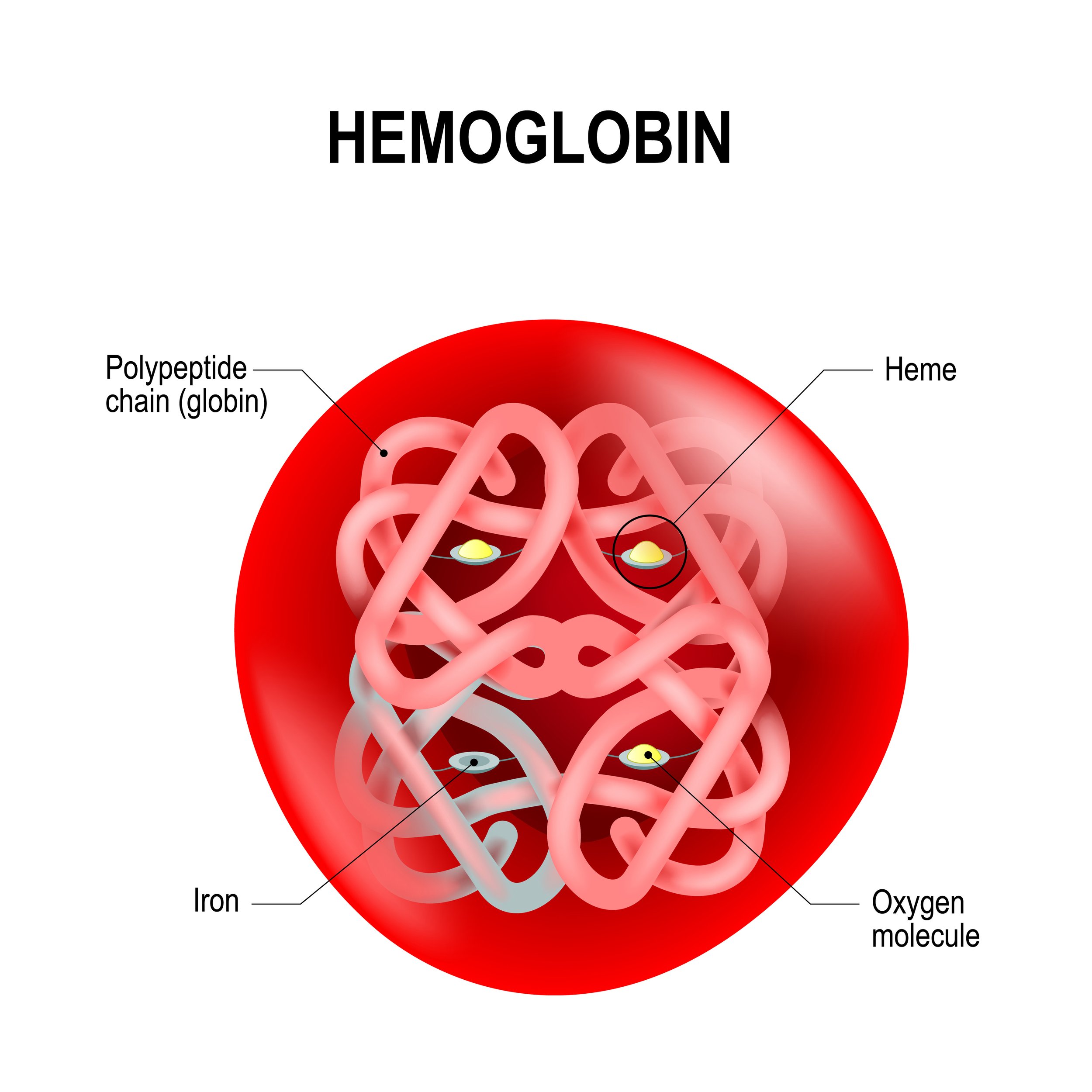
Extracellular vesicles are nano-sized particles that circulate in the blood, are secreted by all cells, an contain microRNA. Photo by Dr Rachael Dunlop.
Researchers at the Brain Chemistry Labs in Jackson, Wyoming, reported today in Brain Communications that they have identified an ALS-specific biomarker, an “ALS fingerprint,” in the blood. The biomarker of eight microRNAs (miRNAs) can be detected via a simple blood draw.
Using next-generation sequencing and real-time PCR, the team analyzed blood samples from patients with ALS, Primary Lateral Sclerosis (PLS), Parkinson’s disease (PD), and healthy individuals.
The eight microRNA ALS fingerprint accurately detects ALS with as high as 98% accuracy and can separate ALS from PLS and PD.
“Faster diagnoses will allow for earlier treatment, which will improve patient outcomes,” says Sandra Banack, lead author of the study.
To confirm its reliability, the biomarker was tested across four different patient groups, in two labs, with various technicians and collection methods. The ALS fingerprint consistently produced reliable results.
Researchers believe this blood test could assist neurologists in diagnosing ALS and complement current clinical assessments.
Dr. Paul Alan Cox, Executive Director of Brain Chemistry Labs, hopes to secure a diagnostic company partnership and make this test widely available to neurologists within 18 to 24 months.
————
Brain Chemistry Labs is a 501(c)(3) not-for-profit organization in Jackson, Wyoming, that seeks to discover new ways to prevent, diagnose and treat ALS, Alzheimer’s, Parkinson’s and other serious brain diseases.
The Brain Communications paper, “A microRNA diagnostic biomarker for amyotrophic lateral sclerosis” (DOI 10.1093/braincomms/fcae268) can be accessed here.